A blog started in 2013 to inform family and friends about my treatment and progress for early breast cancer. Then I went and got two brain tumours,,both GBMs, completely unrelated to the breast cancer, so the blog continues.
Background and overview
Tuesday, 31 December 2013
New year, new things to learn
Bloods
Ending the year with a bang
Monday, 30 December 2013
Another sleepy day. It's so hard to wake up once I've fallen asleep, my body feels like a log, and it's only the fullness of my bladder, the cold pain across my head, or the awareness that I should be getting up to eat and take my medications that forces me to rouse myself. Otherwise, I could be like Snow White and sleep deeply for ages. I don't know if I'd be happy to be woken by Prince Charming, I'd be perplexed and disoriented
I found this article recently, and it rings true to me.
Though I find that thinking of the things I regret only makes me miserable, angry, and frustrated that I may not be able to rectify the infinite number of mistakes I can generate. It's more healthy to forgive myself, to cherish myself for doing the best I could most of the time, and to focus on doing the best I can, with a calm, loving, compassionate, joyful and grateful heart in every moment from now on. I won't get that right every time, but if I practice, I should get better.
Two weeks after brain radiation finished
School holidays have begun, and the first day hasn't been too bad. I'm thankful that my old housemate, Debbie (Barkly St, Carlton, 1990-1995), has been here since Tuesday, she's fed the boys and kept the house running while I've been feeling very lacking in energy. I am still a bit surprised that she came on Tuesday, and that it's Friday and she's gone already. We had lots of good conversations, as old friends do, but the time has gone in a blur.
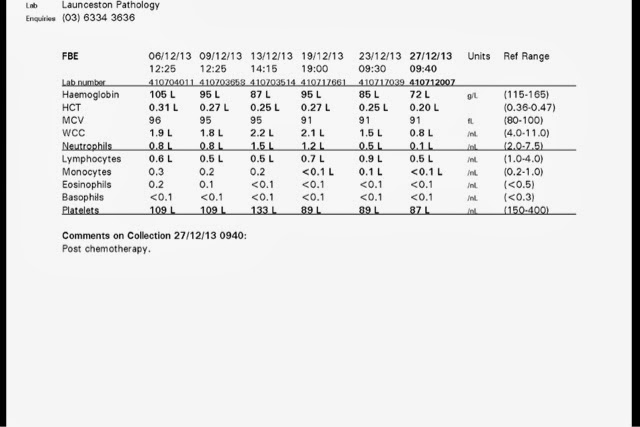
I was still neutropenic when my bloods were taken on Tuesday - neutrophils stable at 0.8 - so until my bloods return to normal, I won't be starting the chemo that was supposed to start next week.
Today I was awake most of the morning, had a nap from 11ish to 1pm, when Mum woke me to remind me to have lunch, and then gave us a lift to the city (via the Pathology Lab, for my second FBC this week), to watch Cloudy with a Chance of Meatballs 2. The movie was okay, my main reason for going was to see if I could tolerate a movie, because I'm very keen to see The Desolation of Smaug with the boys after Christmas. I'm pleased to report that I was able to see and follow the movie today, I didn't get too tired, and the second Hobbit movie should be fine.
I read to the boys until they fell asleep last night, and stayed an hour later because I couldn't put the book down (Cressida Cowell's How to Train Your Dragon Series : How to Betray a Dragon's Hero - absolutely brilliant! Amusing for adults and children, with complex long-term plots and moral dilemmas, more fun and less stodgy and dark than the later Harry Potter books (dare I say it?)). They let me sleep in until 8 this morning, which felt like a treat, and Debbie made me a delicious omelette.
My blood pressure has been a little low this week, causing me to feel dizzy and unwell if I stand up or sit in a chair for too long, and I feel like Raggedy Anne, or the Flippy Floppy Scarecrow from PlaySchool. I should be getting a half-hour walk in each day, but I'm not sure I'm achieving it. It's just so hard to get out and walk with my energy at such a low ebb, and the dizziness doesn't help at all. My rad onc put me onto something to help with the low BP. and I'm trying to drink as much liquid as possible - I'm told that coming of the dexamethasone can affect BP. At least I have Ben and my doctors telling me to wean off the Dex slowly - reading various forums on the internet, some patients have gone off it quickly, and have very unpleasant experiences - it's actually dangerous to go off Dex quickly, because the adrenal glands need to start producing cortisol naturally again. I can't reliably remember the details, but if you're interested, look up Addisons disease.
http://en.wikipedia.org/wiki/Addison's_disease
Oops - reading that, maybe my symptoms are related to coming off the dex.
Corticosteroid withdrawal[edit]
PS - (30 December) - well, I'm glad it wasn't an addisonian crisis, just a developing pancytopenia, hopefully secondary to chemotherapy and bone marrow suppression. 3 units of blood down, two more tomorrow, then hopefully the old bone marrow will wake up and start producing cells again. Time to sleep.
goodbye, good riddance, and thanks for the lessons, 2013!
The boys are finally in bed, and I'm getting a little time to myself in my bed. There's so much I want to write about, I'd need a few hours to do it all.
I had another blood test this morning, my neutrophils are still down in the severely neutropenic zone, my platelets are up a bit, but my haemoglobin is less than 80, so it's another two units of blood for me tomorrow. I didn't realise (never needed to know before) that whenever you have a blood transfusion, they need to take some blood for cross-matching, just to make sure they don't give you the wrong kind. I didn't realise I had the form for cross-matching in my bag when I went for the blood test this morning, so it has to be done tomorrow morning at 8, then my transfusion starts at 9. My poor veins! they can't use my left arm because of the lymphedema, so there are only two or three in the right arm that can be used, and I've already had a sample taken this morning and contrast injected this evening. I hope they hold up to giving the sample tomorrow morning and being cannulated for the transfusion. I've lost count of how many blood tests I've had this year. At least I seem to be getting very skilled nurses lately, the last dozen have hardly hurt at all.
The last few days have been good, my New Year's resolution of seeing or talking to people is working out well, and it isn't even 2014 yet! I've had a number of enjoyable conversations with friends in Melbourne, and three visits from friends and family. It's so good to see or speak with people, and the shared laughter is wonderful. I'm going to try to call people more, and read depressing news stories less, in the months ahead. The only downer is that I get tired quickly when I'm talking, I can feel my attention wandering, I worry that I'm repeating myself, and I feel slower in my thought processes. I'm sometimes able to be quick and witty, but I feel like my thoughts are swimming through custard at other times. I wonder if it's related to the pancytopenia?
When I was having the combined chemo and radiotherapy, the fatigue was more physical, and it came over me like a giant wave, or as if someone had just pulled the plug on my energy reserves. When my haemoglobin was falling, my arms and legs started to feel weak, like a rag doll with the stuffing slowly being removed. I'm used to that now, the transfusions have helped a little, but the nausea, lack of appetite, dizziness, and shortness of breath on walking are not pleasant.
I'm feeling a sneaky sense of satisfaction for managing to put away a couple of boxes today, and to have tidied up one small corner of my bedroom - I haven't managed to do much for ages, so it was a real achievement to see something that could be done, and to sprint in and do it.
I've been typing for 30 minutes now, and my arms are feeling heavy. I don't want to go to sleep, there are so many things I want to share - how beautiful our garden looks, the cheerful songs of the birds at 430am (first light), how this year has taught me to be calmer and more grateful for all that I have, how my calmness is slowly causing changes in my boys, how much I love them and want to be with them for many years ahead, how I keep hearing of more and more people with GBMs who have lived for many years (and, conversely, how survival seems dependent on location of the tumour, age of the patient, and what healthcare system they're in. If the tumour is inoperable, the patient over 60, or the healthcare system highly privatised, many people do not get treatment (surgery futile/too risky, treatment too likely to impair quality of life, chemo and radiotherapy too expensive).
I'm too tired to be worried about the results of my MRI scan. I'll wait for my rad onc to tell me. I'm too tired to worry about all my things sitting in boxes and filing cabinets at work. The people at work will look after them for me. I don't have the energy to worry about what my bone marrow is up to. I need to support it with rest and nutrition, and to avoid getting infections. I'm nearly off the Dexamethasone, and also the Sodium Valproate (Epilum), so I will hopefully feel a little less muddle-headed when they're out of my system.
My plan is to spend my time looking after my physical, emotional, and spiritual health, to care for my family and friends (as much as I can while my bone marrow limps along), and to one day be able to improve things for people with brain disorders, and brain tumours, and their families. I don't think I'll be turning this blog into a book - I have more important things to do than edit it for that purpose - a blog is accessible for whoever wants to read it, whereas books cost money, and I'd rather this be a gift for people who may benefit from it. I'll just have to check it over before I lift the privacy restrictions to make sure I'm not violating too many family secrets (I think I've been careful, but it's worth double-checking).
I'm blessed to know all that I do about the brain, and to have had tumours in areas that haven't caused major problems with memory, language, cognition, or physical abilities. For people without my background in neuropsychology, however, coping with changes caused by their tumours, understanding the literature, and navigating through the system must be incredibly difficult. I feel like we've been fighting battles all year, the first was to get through the breast cancer treatment without succumbing to an infection, the second has been to get through the fatigue caused by the combined radiation and chemotherapy, and now there's a third, unexpected battle, of dealing with my suppressed bone marrow. I might start getting regular gcsf injections if things don't improve.
I so hope that 2014 will be a better year, for everyone. Peace, love, and good health to all of you.
Wednesday, 25 December 2013
Christmas update
I'm lying on the couch in the family room, resting, and everyone keeps asking me if I'm going to go to sleep. I don't feel like I need to sleep right now. I had a good sleep last night, after a good nap yesterday afternoon. I'll sleep when I want to and need to. I need to write just now.
Our Christmas was nice and uncomplicated. The boys were up early and hoed into their Santa stockings, then spent the day building Lego (followed by tantrums today when their mildly autistic cousin broke part of one). Mum had brought food over the day before Christmas, so all we had to do was roast a chicken and some veggies, and put the food on the table. Everyone was happy with the selection, and Mum was very happy to take home some leftovers. The only downer was waking up and realising that it was our second Christmas without Dad, and remembering that Ben and I had thought that 2013 couldn't possibly be worse than 2012 was. We're just wishing for 2014 to be better now, and are not making silly statements that may tempt fate.
I had my bloods taken (again) on Monday morning, and got a call from my rad onc, saying they'd fallen again, and that he'd arranged for me to see a haematologist on Tuesday morning. The clinic then rang me to ask if I could see her at 2 that afternoon. My haemoglobin had improved after the transfusion, but everything else is still low, or trending downwards, so I now have a pancytopenia (white cell counts, neutrophils, lymphocytes, HCT, and platelets all low). She's ordered some additional blood tests for Friday (PEP/IEP: quantitative Igg, B12, folate, and iron studies), and I'm not to take Valcyte again until we see if my bloods recover. It could be that the Valcyte is suppressing my bone marrow. If my bloods don't recover when I'm off the Valcyte, and if they can't find another cause, then I may have to have a bone marrow biopsy.
I love my haematologist, she's a wonderful woman with a fantastic manner, though I'd prefer to be working with her in the clinical school, where I used to do sessional lecturing to the medical students. It was slightly discombobulating to hear her say that she had been following my progress over the past year, given my "crashing neutropenias" and "rapid nadirs" - it turns out that I'd been discussed at the oncology meetings, and that they've been wondering if I have a genetic or immunological predisposition towards having a poor bone marrow response to chemotherapy. Great! It's so lovely to be special. Even before my brain tumours were discovered, I was an unusual patient. Apparently not many people respond to breast cancer treatment as I did. It probably wouldn't have made any difference to me if I'd known at the time. It was just something I had to get through, just like this is.
So I'm trying not to worry about things until I need to worry about them. I'll stay off the Valcyte until my bloods recover. If they don't, I'll have further tests. I may need to have "bone marrow support" with gcsf shots, and I guess the results of my bloods will determine if I restart the Valcyte, and if, or when, I start the chemotherapy with Temodal that was supposed to start last week.
In the meantime, I'm enjoying being at home with the boys in the school holidays, and am looking forwards to seeing the next Hobbit movie with them tomorrow. I'm trying to avoid the sugar and carb-laden Christmas treats in the house, and to follow the ketogenic diet for cancer, though it's hard to prepare food when you feel nauseous and don't know what to eat. I enjoyed the pad thai that Ben brought home from the takeaway today, so I saved some for dinner - not on the diet, but tasty.
I'm also meditating and imagining myself healthy and cancer-free whenever I get the chance. I'm feeling more peaceful and less irritable as a result, though Ben says it might be because I'm nearly off the Dex and my Valproate (Epilum) dose is going down (killjoy!). My face is still puffy and has fuzzy hair around the sides, but I don't care. I don't look in the mirror much any more, I'm just happy to be alive. Doctor Who is on tonight, we're seeing the Hobbit tomorrow, and although this year has been tough, I've grown and learnt to love myself and others better than I did before.
Love is the most important thing.
(I just wish I could have a fairy godmother to come and clean up all my clutter, and sort out all my papers and electronic files! I've set these tasks aside for later, when I'm well, I know they're not as important as getting better, but they're still something I don't want to worry about… I think the worry is a well-suppressed fear of dying without all my photos, presentations, lectures, and useful files saved in a format that others might be able to access. I feel a responsibility to the family name to leave a legacy behind, to make sure my life has meant something, to help people. Ben says I'm being grandiose and sentimental, maybe he's right, but I've always been like this)
Is Human cytomegalovirus (HCMV) the reason why I got two primarycancers in one year?
I'm feeling much better after Tuesday's blood transfusion. It helps that the boys are on holiday - I have slept in until 930 yesterday and today, and they've played happily together.
I've been doing a little research this afternoon, and found some articles which propose a viral link with breast cancer and GBMs, and one which claims to refute it.
I haven't found anything on Valcyte and breast cancer, only warnings that Valcyte can cause cancer and shouldn't be used in people with bone marrow problems, or who are breast feeding. Why can't there be an effective and innocuous drug to treat cancer? I'm going to try to work out how to do the ketogenic diet properly, it seems to be the safest option, both as an adjunct to conventional therapy, and as a backup in case the conventionals don't work for me.
Thursday, 19 December 2013
Tuesday, 17 December 2013
On being an ill health professional, and married to a doctor to boot!
I had a good long chat with one of the nurses today, including about the challenges of being a patient when one is used to being a healthcare professional, and on how doctors' family members can get treated differently from other patients. I found this interesting, though somewhat wordy, article, about the issue of dealing with "physician-patients" or the family members of physicians.
http://jama.jamanetwork.com/article.aspx?articleid=188281
It fails to mention findings from the clinical judgement literature on a tendency of clinicians to not want to come up with potentially bad diagnoses in patients with whom they identify, such as other clinicians, or the partners of their colleagues. This is particularly difficult in small communities, when many health professionals know each other.
A suggested solution to this impediment to clinical judgement is for the clinician to recognise when they identify with the patient or the patient's partner, and to evaluate if it may cause them to be not as vigilant as usual to clinical symptoms or signs; to always go through the same diagnostic procedures for every patient, no matter who they are; to consider all diagnostic options and rule them out methodically, particularly the worst case scenarios; or to pass the patient on to another colleague.
An interesting thing from the article, for me, was the comment that physicians often minimise, downplay, or misdiagnose their symptoms. I know I've been guilty of that, and I'm just a neuropsychologist with a dangerous amount of half-knowledge. I can talk the talk, but I don't have the knowledge to back it up. It's very hard to stop talking the talk when I see a doctor and treating them like a colleague, and ask them instead to pretend that I know nothing, that I'm just an ordinary patient, and that my husband knows nothing as well.
Saturday, 14 December 2013
More good news on valcyte.
Simple truths
I've been incredibly tired, and have needed lots of sleep, or at least rest, during the day. It's so unlike my former self, to not even have the mental energy to read things for long, I've had to give up my expectations of myself as a kind of Super Fi-Fi and accept that there is some kryptonite around that is sapping my energy, and that fighting it will only take more energy. I need to be smart and work out a way around it.
My sleep at night hasn't been as disturbed as in the past, partly because I'm trying not to stay up too late compulsively reading about ketogenic diets for cancer, or other treatments. I've also help back on blogging, because it takes time and has left me feeling a little exposed at a time when I need to conserve energy.
Letting myself rest, physically, intellectually, electronically, has led to some interesting and important insights. I will list them, and expand if necessary.
1. I woke up a couple of weeks ago realising that it wasn't a criticism when I was told that I was "sensitive to criticism" back in 1983. It was a simple statement of fact, and I'm sad and ironically amused that it took me 30 years to realise that if I continue to be my own greatest critic, then I'll always be sensitive to perceived criticism from others, leading to defensive responses to perceived hostile comments or vocal inflections from family. It's so good to let go of that need to criticise and flagellate myself, and to believe that I'm loved and worthy of love, and to finally allow myself to love myself. I dared not do so before, lest I be guilty of the sin of pride, or, as people told me as a child, getting a "big head".
2. There is no substitute for real-time, real-life interaction with other people, especially close friends and family, either in person or on the telephone. The laughter, sense of sharing, and spontaneous, unedited conversation is infinitely more satisfying than the artificial interactions had via electronic media, though the latter do have their place, as long as it's not the only kind of social interaction you're having.
3. I've been feeling lonely lately because I've not been getting enough real-time interactions with family and friends, so I need to rectify that situation. I will call you, or you can call me, and even if we play phone-tag for a fortnight, we will have a good chat at some time. I want to hear about what's happening in your life. I'm sure it's far more interesting than mine.
4. Social media like Facebook can give an illusion of community and connectedness, but after spending too much time on it over the past year, I feel like a shallow voyeur into other people's lives, and while it's lovely to see your babies, children, weddings, and pets, it doesn't give me the emotional connectedness I get from having a good yarn with someone. I am going to spend less time browsing Facebook and more time calling people on the telephone, or arranging cups of tea.
5. Thoughtful emails, texts, or cards. that expect nothing in reply are appreciated. As are responses to my response, which say "you didn't need to reply"
6. No insult intended to anyone, but there are people in our lives who are much closer than others. For me, I've realised it's an intimate circle of people who I can rely on to listen and support me when I'm feeling completely despondent, who can make me laugh despite myself, who can help me see there's always light at the end of the tunnel, who help me to accept, forgive, and love myself, and to remember that I am, and always have been, doing the best that I can. I still enjoy the contact, company, and friendship of colleagues and acquaintances, but I now know the difference between the truly close friends and those who aren't. I'm still processing the realisation that my blog has given a wide range of people access to more personal revelations and reflections than I would normally share outside my inner circle, (making me feel a bit exposed), but I've always worn my heart on my sleeve and tended to excessive self-disclosure, so this blog is an authentic reflection of myself, and people's positive feedback (mostly when I post links to it via Facebook) has been a validating experience.
7. I've spent a large part of my life trying to achieve a sense of self-worth and belonging through my career as a neuropsychologist, and through trying to help improve things for people with brain disorders through training, educating, supervising, and sharing with other neuropsychologists. I believe these are worthy goals, and I think I was reasonably good at it - given the positive feedback I received from colleagues around Australia during my time on the CCN national committee and as a frequent poster to a neuropsych mailing list. However, I was beginning to suspect that I was sublimating other emotional needs in pursuing those professional goals. Now that I have learnt to love and accept myself, I know that I don't need the approval of others to feel good about myself. I can generate that love from within. It feels like a warm, golden glow. Comfortable, self-sustaining. Not the sugar-rush of compliments or appreciation of others, that light up the furnace from outside, but quickly fade away, and need another good deed to elicit another sugar-cube reward. When I get over this tiredness, I hope to have a self-sustaining, gently-burning inner furnace that will allow me to live and love well, and hopefully have some time and energy to give to helping people outside my family. At the moment, however, I need to look after me and my family first.
8. I realised that a lot of my quarrels with Ben and Mum were over the use of language - I have a bad habit of correcting their pronunciation of words, or of trying to clarify what they mean, or of trying to help them express themselves more elegantly. It's like I'm a self-appointed grammar editor, and it must be really annoying to them, even though it's well-intended on my part. This realisation came to me in the shower the other day, and it took a while to work out why I did it. I remembered that I'd been afraid of public speaking at school, which wasn't helped by being put into the school debating A team on short notice in year 12 for my first ever debate. I was the third speaker, and was so afraid I was going to humiliate myself in public, I could see everyone in the audience looking at me in pity. Some members of the opposing team, from a 'tough' school, came up and expressed their empathy for how nervous I was. At Melbourne Uni, tutorials and college dinners, or even friends' rooms, were dangerous places to mispronounce words or to express oneself inelegantly: these were often met by raised eyebrows, sniggers, derision, or interrogation about what exactly you meant by that statement, making me want to fall into a pit of shame and disappear under the table. So my irritating attempts to help improve the pronunciation of words or clarity of expression in Mum and Ben (I hope not others too, sorry!) has been based on a desire to protect them from the embarrassment I felt at Uni, particularly as a fresher from quaint, provincial Tasmania, in 1986. I'm going to try to curb my automatic editorial tendencies, and hopefully cause less arguments. It doesn't really matter that Mum says "comfortable"differently from me, or that Ben and I differ in the pronunciation of "ubiquitous" - just because I like the sound of my way better doesn't make it right (well, I might be right, but it doesn't really matter, it's not like I'm giving them a pronunciation test). And trying to correct them just creates bad energy when we could be having a good conversation.
9. A good sleep, and dreams, are wonderful ways to improve mood.
10. Children, even those aged 9 and 11, aren't that good at recognising when they're hungry and tired, and need to have food provided at regular intervals to reduce potential emotional volatility, thus improving the general level of happiness in a family. I suspect the same may apply to husbands… and wives.
Time for my bedtime melatonin capsule, and some panadol, and sleep. I hope the boys sleep in tomorrow morning!
Sunday, 8 December 2013
Blood, Pollyanna, and Harry Potter
I've had red carpet treatment at Launceston pathology the last few times I've been there. I will try to see this as a good thing, not as a sign that I'm becoming a 'frequent flyer'. The receptionists are starting to recognise me, ask if I want a 'senior collector', and direct me to a special waiting area.
The nurse uses a small gauge needle, and gets it done very quickly and almost painlessly. Have to protect those two veins in my right arm, at least until the twice-weekly blood tests are over. One of the veins was starting to retreat from their needles last week, and I can't give blood on my left, thanks to the lymphedema.
It's not too bad, thankfully, and wearing a pressure garment on one arm isn't that uncomfortable.. It would be far worse to have to wear pressure stockings for leg lymphedema
Gee, I'm so glad I read Pollyanna as a kid, and have had so much practice in looking for the good in everything, the silver lining to every cloud. It's a habit that keeps me from falling into self-pity, even though it reminds me of the Secret Seven and the Famous Five- children keeping on against the odds, without adult help, beating the bad guys. I wish I could say I had amore sophisticated coping strategy, but it works, so I won't knock it.
My situation is a little more complex than Pollanna or Enid Blyton, and not quite on the scale of Harry Potter, but I sometimes feel as if I'm under a Dementor attack, and that I need to cast the Patronus Charm to stop them from sucking the happiness out of me.
It's amazing how powerful happy memories can be, and the feeling of being loved by others. JKR captured some true magic in the Patronus Charm (and I find the thought of being saved by Remus Lupin, or Surius Black, quite pleasant ;) After the Dementors have gone away, I'd just like a nice stay in sick bay, until I'm all better again. Then let me fly a Hippogriff!
Wednesday, 4 December 2013
is it socially acceptable to be a bald woman after treatment for cancer?
The only downside to the weekend: the realisation that my idea of being able to comfortably be a bald-headed woman in public is possibly a fantasy. We had Nathaniel's birthday party on Friday, and my hat was too hot for the venue, so I took it off, exposing my recently clippered scalp. Most of the kids (9yo boys) didn't give me a second glance, one or two looked curiously, but they all came and thanked me at the end and gave me lovely smiles. The mums who I knew were fine about it, and we conversed normally.
I spoke with two of them about a set of homework projects that had been set for Year 2, and confident that I now had spoken to more than 5 parents who have issues with it, I asked a new mother what she thought, making the mistake of saying what I thought first, perhaps a little too passionately. She said that she and her husband had found it required a lot of work, but that it was interesting for their son, and allowed him to bond with his father. I silently envied her non-working mum, healthy family situation, and then had the sense, for the first time in my life, as being looked at as someone who was somehow disabled - the passion and intensity that I have applied to so many things over my life seemed to be interpreted as signs of a dysfunctional brain. She avoided me for the rest of the party. Caroline (my cousin) later said I seemed to come on a bit strongly, which brought tears to my eyes. I don't want to scare people away - I've spent all my life trying to be kind to people, and to engage them, and make them feel safe. It feels like a failure to have stuffed up - I should be able to ask someone for their opinion and not get too passionate in expressing a contrary one.
I've become more passionate about a whole lot more things lately - climate change, asylum seekers, and political corruption in particular. Perhaps because I'm not working and I'm thinking of the future for my boys.
I've always been good at unintentionally reducing my mother to tears over silly little things, and now that I've had brain surgery, I'm trying hard to avoid it, but not successfully. Old pattens are hard to break, and I worry that people will see any irritability on my part as a sign that I'm cracking up or mentally unstable.
Writing that, I worry that I'm becoming paranoid. But I don't think people are out to get me, I just worry that people won't understand that my irritability or poorer concentration are because I am so tired, I can only focus on one thing at a time, that I'm painfully aware of how fragile life is, because I'm undergoing radiation and chemotherapy, because I'm on steroids. I'm worried, like many of my patients before me, that people will think I'm crazy.
How ironic! The neuropsychologist who prided herself on giving feedback and educating patients and families is anxious that others will think she's crazy. She knows she's not, but there are so many people to educate.
When I mentioned the bald headed thing to Ben tonight, he told me that I shouldn't bare my head in public, that it's too confronting for people, that I shouldn't let my ideology (that people with disabilities should be able to be accepted in public) override social sensibilities. Unfortunately, that irritated me just a little, and I had to remind him that men often make the mistake of giving women solutions to problems when women just want to talk to men about their feelings, which helps them to come up with their own solutions. Which is why I blog. I think I might need to talk to someone at the Cancer Council about this though, they'll have experience with it.
Maybe it's the scars on the head that do it. People are used to puffy faces, hats and scarves in cancer patients, but for women to reveal the bald head is possibly too confronting. One of the radiotherapists said she used to get funny looks and even calls of "dyke" from passing cars when she shaved her head for charity. I've had some funny looks when I've been walking with my forearm crutch - at times I can get along at a good pace, but at others I'm so tired, I need to lean on it. I won't be walking outside with a hat off, because it's either too cold, or I have to keep the sun away. But why can't I be bald inside? Why should I be ashamed of my baldness and scars? I feel fake wearing wigs, and if we hide disabilities, it just stops people overcoming their fears and recognising that all people are the same.
An interesting lesson in how much courage it can take to accept one's changed appearance and capacities and to not be afraid of showing it to the world.
Oncology review #1
The plan seems to be to gradually wean down the dexamethasone every 5 days. So after being on 2 mg in the morning and 1 mg at lunch, I drop the dose to 1.5mg in the morning (mane) and 1mg at lunch (midi) for 5 days, then 1.5 mane and 0.5 midi for 5 days, then 1.0 mane/0.5midi, then, I guess, 0.5 mane and 0 midi for 5 days, and then, hopefully, no more. He said that the "hypomania" I experienced when I was on the high doses of Dex may swing the other way when I'm off it. I'm proud of myself for not growling at him - I know I seemed hypomanic, but I don't believe my euphoria and elevated mood was purely steroid-related. I was so happy to be alive, so excited to have dodged a very bad outcome, it wasn't all the Dex, though I suspect the steroid helped me to think and talk faster than usual. Since the surgeries, I have gathered enough inner stores of love and happiness from this year, and my whole life, that I'm confident I'll be able to get through any dark days ahead. If I'm feeling down, I'll get on the phone to friends and family, so watch out! Talking and laughing with you will be all the therapy I need.
When I'm off the Dex, my puffy face with the fine hair around the edges might then return to normal, not that it bothers me. I don't look in the mirror that much, not having any hair to worry about drying, though what I've seen of the regrowth is pretty amusing. I'll get one of the boys to take photos to illustrate the fascinating pattern that conformal radiotherapy to two different areas via 9 different approaches has achieved. If the hair doesn't grow back over the RT entry and exit spots, I'll have to keep it shaved - there's no way I could grow enough hair to cover the bald spots, and I've always loathed the comb-over look. So it looks like I might get to be a bald woman after all. I don't think I'll do it often in public - it's cold, I need to protect my skin from the sun, and I'd like to avoid the pitying or curious looks of others. In certain situations, it might be fun to be bald, but I think it would be more fun to whip off my hat or scarf and show off the battle wounds after demonstrating that a person who has had brain surgery can still be normal. I have tried my wig on, but it isn't comfortable, and I feel like a fraud. I'll have to see if I can get a refund, I've only worn it once. I have a number of lovely scarves that I can tie quite well, and a collection of hats. With the headgear on, no-one will know what kind of cancer I've had, and there won't be any prejudgement about the state of my cognition from the scars on my head. Oh! I'm still concerned about how others see me, aren't I? Hard to give up the habits of a lifetime, and look at how good I am at rationalising them! I will go bald in public some times, it will just depend on the context and how I feel.
What else did my lovely rad onc say? (I'm writing this as much as a record for myself as as scintillating information for you, dear reader).
Three weeks after the RT finished, I start chemo again - as long as my bloods are normal. This will be with a lower dose of Temodal, again in capsule form (I don't know if my veins could cope with more infusions). Six cycles of chemo: 5 days on, 21 days off. My white cells had dropped from 1.2 to 0.7 yesterday, possibly because I have a cold, and there's a risk of bone marrow suppression again, partly just due to the drug itself, but also because I'd had the 6 cycles of FEC-D for my breast cancer. Lucky me! All I can do is get a good mix of rest, healthy food, and exercise as I can, as well as laugher and love with family and friends, and keep on going.
MRI usually takes place after the complete course of treatment is over, but we can do mine earlier, on the understanding that we don't do anything if there's pseudoprogression (Psp) (where it looks like the tumour has progressed, but it really hasn't). I've done my reading on Psp, and it seems they know how to tell it apart from true progression, and it's even associated with better outcomes, so that's fine by me. I'm more concerned about new nasties lurking in other parts of my brain. I hope there aren't, but I'd rather get them out when they're small and manageable. I sometimes have word-finding difficulties, and have been dropping things with my right hand lately, which is probably just due to my general myopathy and being sensitised to looking for anything abnormal, but I'd like to be sure that there are no new surprises in store, like something growing in my left temporal lobe. Feeling like a hypochondriac again, must not feed the fear.
I saw my breast surgeon for a review last week (all okay), and she wrote a referral for a repeat mammogram and ultrasound to be done in January. I'd prefer to just have a breast MRI, as it's less painful, there's no ionising radiation (I've had more than my fair share of that this year, I think), and I thought it was more sensitive, but my rad onc said that a mammogram would still be needed. I'm happy to have an ultrasound, I just hate mammograms. Drat. It's so uncomfortable, though at least there's just one breast now, so only half the time and discomfort.
Time to sleep. Sweet dreams.
Things to say to people with cancer or illness
http://www.mamamia.com.au/health-wellbeing/response-to-mias-what-to-say-to-sick-people-colum/
scary diagnoses and patient education
Dear colleagues
If, like me, you have always been interested in knowing about the brain, you may have found some conditions too horrendous to contemplate because of their reputation for rapid and terrible suffering and mortality. For me, these conditions included CJD (which I saw rapidly consume the 48yo mother of a beautiful Indian bride) motor neuron disease, advanced Huntington's disease, behavioural variant Frontotemporal dementia (especially heartbreaking to see it steal a 22yo new graduated mother, and how it destroyed the family of a loving 36 man, who had taken sides on what appeared to be a pending divorce before the diagnosis became clear. Aggressive brain tumours are also in my feared conditions list - they have the power to kill rapidly and efficiently, and median survival outcomes seem dismal.
To help demystify one of my top scary brain disorders, I would like to recommend the following article to you.
http://neurosurgery.ucsd.edu/glioblastoma/
It is excellent. It provides hope through the use of calm, factual, plain English, without the emotive drain of survival statistics.
Good for cutting though the fear of death and disability.
We need to cultivate hope in our patients and their families. Even if a diagnosis is grim, there is always hope. There will always be love from family and carers. There can be dignity in disability. That is, unless we put our fears in the way, then we minimize the potential of the patient and family to make the most of the situation they are in. We're not helping the patient in such a situation, we're dealing with our own fears of death, loss and suffering.
Monday, 2 December 2013
One week post radiotherapy
Monday, 25 November 2013
Happy day
Whoo hoo! I finished radiotherapy today. The sense of relief is like completing HSC, Uni exams, my honours thesis, and my PhD rolled into one. No more cancer, no more radiation, just rest, exercise, healthy diet, and a few
Cycles of low dose chemo to go. The next half of my life begins today :)
Two zaps to go
A few of you have written lovely long emails, which I haven't had the energy to respond to - know that it's wonderful to hear from you and your thoughtful responses to my blog, it's good to know who's out there. In response to one question, the fatigue has been pervasive and different to what I felt during my breast cancer treatment. I didn't need to sleep during the day so much then, except when I was in hospital with neutropenia, when a brief morning and afternoon nap sufficed. Since the initial exhilaration of having survived surgery for two brain tumours and the corticosteroid-induced sleeplessness and high energy of the first month after sugary, I've had waves of fatigue come over me, which I've sometimes foolishly resisted, and later paid the price with increased irritability or fatigue the next day. I find it very hard to sit or lie still and do nothing, apart from compulsive reading, which isn't really resting my mind. I don't watch much television because it is inane rubbish during the day, and I've started to take great delight in muttering comments back to the morning presenters while I wait for my treatment in the Holman Clinic (mutters facilitated by the presence of my cousin Caroline, who helps it become a very funny experience). I'm loving the Dragon Riders of Berk series on the ABC, and am very excited to find that there are two series on YouTube, so I guess if I get the right kind of programs (funny fantasy or science fiction), I can lie down and watch TV to rest.
There's still the problem of wanting to de-clutter the house, and not having enough energy to do it. I am motivated to do it because I feel a strong sense of stagnant energy from the accumulated clutter in our house (books, papers, boxes in particular). When we visited my cousin's yacht in Hobart, I could see the appeal of going away with only the things you absolutely needed, as there is no room on a yacht for extra things. If I could wave a magic wand and make everything that we don't need disappear, I'd be very happy (thanks, CL, for that idea). From reading my old Feng Shui books, if improving the flow of energy can make a difference to people's health and relationships, then I'm very keen to do it. I know that Feng Shui may sound like superstitious nonsense to some, but I've been interested in it for years as a lot of the principles make intuitive sense to me. Like having a bright and welcoming entry to your home, and not having accumulating unused or broken things, or clutter (are you seeing a theme here?).
I was stressing about the lack of progress on decluttering yesterday, and Caroline said something very wise and helpful: "There's no hurry. You've got all the time in the world to do it. Once your treatment is over, you'll start to get more energy back, and you'll be able to do a little bit more each day." Ben managed to clear out a lot of clutter from our back hallway (shoes, bags) today, Caroline cleared off the dining-room table (a magnet for papers) and Ben found a blue birdbath that looks wonderful in the garden outside our kitchen.
Caroline knows me so well, she sensed that I fear there is some deadline to do all this, that tidying up the house and getting my affairs into order is an important thing to do. It's good to have her remind me that the most important thing I can do is look after myself, get the rest that I need, and not feel annoyed with myself for not having the energy to do the amount that I used to be able to do. I have all the time in the world. I am going to get through this.
http://www.sarahmamalai.com/
The boys played beautifully today, lots of laughing, no fighting. The routines and consequences that I've been putting in place are working well - for example, they can't play an electronic game until they've showered and dressed in the morning. They can only play for 30 minutes in the morning or afternoon; if they don't stop before or at the allocated time, they lose playtime in the next play period; they need to read or do chores before they play in the afternoon. Whining, pleading, yelling, and other unpleasant behaviours intended to help them get their own way get counted using the 1-2-3-Magic system, which is resulting in impressive results.
I have much more to say in my head, but need to rest now. Take care, and keep in touch.X
Sunday, 24 November 2013
Don't get down over median survival times, the data is skewed!
In fact, I'm quite angry that there aren't enough patient-oriented sites that overcome the pessimism and despair that the medical literature probably engenders in people who do not understand statistics. The excessive use of median survival times when talking about cancer probably contributes to depression and hopelessness in patients and families, at a time when they should be fighting with all their might.
To put it simply, the median (where 50% of the population falls) is not always the same as the mean (average). So if 50% of people with a certain diagnosis die within 3 months, then 50% do not, and some people may survive for many years later. We call this a skewed distribution, and in my extensive reading about GBMs, being over 60, having an inoperable tumour or one that can only be partly removed, being physically unwell, and male makes someone more likely to be in the first 50%. Many people die because their tumours are caught too late, or are inoperable, some older patients are not even offered surgery - this data shouldn't be used to create outcome data for all people with GBMs, as it will give an overly negative impression for younger patients and those who have surgery. Ideally, the outcome data should be stratified by age, gender, health status, location of the tumour, extent of surgical resection (full, partial, incomplete), type of treatment given, and should note the duration of the follow-up studies. It's a highly complicated issue, and all patients and families with any kind of difficult diagnosis, like mine, should be able to access educative and hope-inspiring resources, rather the misery-provoking wasteland that's out there.
Luckily, there is an essay by Stephen J Gould that is fantastic, and saves me writing my own. If you don't want to read the whole thing, I'll quote a couple of excellent passages from his essay here, in the hope that it will give you hope for me.
cancerguide.org/median_not_msg.html
Gould was diagnosed with intestinal mesothelioma and survived 20 years, despite the median survival time in the literature being only 3 months.
"Attitude clearly matters in fighting cancer. We don't know why (from my old-style materialistic perspective, I suspect that mental states feed back upon the immune system). But match people with the same cancer for age, class, health, socioeconomic status, and, in general, those with positive attitudes, with a strong will and purpose for living, with commitment to struggle, with an active response to aiding their own treatment and not just a passive acceptance of anything doctors say, tend to live longer. A few months later I asked Sir Peter Medawar, my personal scientific guru and a Nobelist in immunology, what the best prescription for success against cancer might be. "A sanguine personality," he replied. Fortunately (since one can't reconstruct oneself at short notice and for a definite purpose), I am, if anything, even-tempered and confident in just this manner.
…
"The problem may be briefly stated: What does "median mortality of eight months" signify in our vernacular? I suspect that most people, without training in statistics, would read such a statement as "I will probably be dead in eight months" - the very conclusion that must be avoided, since it isn't so, and since attitude matters so much.
…
Monday, 18 November 2013
the restorative powers of sleep
My neutrophils up from 0.1 last Wednesday to 0.2 today, so I qualified for a GCSF injection to boost them, as they've been down for so long, even though I haven't been taking my Temodal since Thursday.
I'm very proud that I haven't developed an infection with almost no white blood cells, but I suppose that staying in bed, at home, has been a good strategy. I really didn't have the energy to do much else, and felt quite pathetic. It was humbling and surprising to see how lacking physical energy affected my ability to stay optimistic - I admire anyone who manages to continue on with a chronic illness or chronic pain. It is so debilitating to feel like you have no energy left, and to fear that you won't regain it. I confess I've been a terrible scaredy-cat at times over the last few days, I was worried that my lack of energy might mean I was going to die, so it's really good to have rallied and to feel my energy building again.
Strangely enough, just like after my surgery, I have an overwhelming urge to do further decluttering in our house - the excess of papers and other unimportant things upsets me. I want my environment to be simple and to only have the necessary things, nothing that's being kept just in case it comes in handy one day.
My hair is going to come off very soon, it is looking ridiculous (the spirals have gone, and there are just tufts of hair left). I'm kind of glad that it might never grow back evenly, I don't think I could cope with fluffy curly hair.
Thanks to everyone who has sent messages and emails. I might not be up and about much, but it's nice to be in your thoughts.
xxx
Saturday, 16 November 2013
Neutropenia, again
I've spent most of yesterday (Friday) and today sleeping in bed. My body feels utterly drained of energy (it's an effort to lift my arms, I feel weak and floppy), and I don't have much of an appetite, though I can eat if I put my mind to it. My bloods on Wednesday showed that my neutrophils were down to 0.1, so I was told to stop taking my Temodal, as it's the only chemotherapy I'm on, and it might be suppressing my white blood cells, though it shouldn't.
I had my RT as usual on Thursday and Friday, and asked on Friday if I should be having my bloods done again, but the nurse, who I hadn't seen before, said no. We got a call at 430pm saying that I should have had them done, and could we come down before the clinic closed to do it. Lucky we live only 10 minutes away, and I have Caroline here to drive me. My bloods haven't improved, but I haven't spiked a fever or developed any other signs of infection, so I'm hoping I'll be able to avoid going to hospital for this neutropenic episode. It's much more pleasant to be at home, apart from having to deal with the kids fighting, and Ben getting anxious that I need to get up and go for a walk so that I don't get blood clots, when the only thing that gets me out of bed is the desire not to wet it. I have never felt so feeble in all my life. When I woke up after sleeping today, I wasn't sure what day it was, or if it was morning or afternoon. At least I know the year, month, and season, and where and who I am, but it's disconcerting to be disoriented to day and time, however temporarily.
I've had some pretty low moments over the last couple of days - feeling so drained of energy makes me realise how much I've generated my sense of hope and positivity from some inner store, and it's hard to get in touch with it at the moment. There's still an ember burning away, and the best I can do is sleep when I need to, walk for short distances outside when I can (once a day) and rest and enjoy the quiet company of family and friends at other times. Pushing myself too hard, or being afraid, is counterproductive, I simply can't do everything I could before. I need to focus on resting and recovering from this 10-month assault on my body.
In January, I described my forthcoming treatment for breast cancer as a surgical strike that would be followed with chemical and nuclear warfare. I had no idea that there would be a second enemy hidden deep within my central command centre that would require two surgical strikes and combined chemical and nuclear warfare, plus a third mopping up with chemicals, just in case. My knowledge of military history is gladly insufficient to allow me to identify a battle of similar stages, but I feel that I have been through a terrible war, and that it will be good to apply the soothing balms of love and peace very soon.
Ironically, my hair, or what is left of it, is growing back thicker, darker, and curlier, than ever before. It could have been fun to have dark spiral curls, though it probably would have driven me mad. Unfortunately, it only covers the back left quadrant of my head now, and will need to be clippered off soon. Even my low level of vanity has limits. I will then become a bald woman, which will make me very easy to identify if I pursue my desired new career of advocacy for people with brain disorders. Nothing like standing out in the crowd.
There are a number of people with different kinds of cancer or brain disorders who have blogs which are public, and which are used to advocate for people with those conditions. I've thought about doing that, and part of me is in conflict about making this blog public now, as I'm told it would be helpful for people going through similar experiences. I have made it private because the initial intention was to help keep friends, family, colleagues, and others updated on my progress. It has been therapeutic for me to be able to write here, and knowing that it's private has allowed me to write more freely than I would if it had been publicly accessible. If I made it public, I would need to edit it, and I don't have enough energy to do that at present. Once I'm stable, I'll start advocating. At the moment, I'll just work on getting better.
Please don't worry about me. They say that the final weeks of brain radiotherapy are the hardest. I'm still here, still very much alive, feeling loved and cherished by so many people. I'm grateful for your prayers and good wishes, and wish I could sit down with every one of you and have a cuppa, or at least a chat on the phone. I just need to get through this last bit and I'll be feeling better. After next week, 3 weeks without chemo to work on diet and exercise, and then the final push. I'll get there.
And in case you're interested, I found that there are two kinds of GBMs: primary and secondary. Primary GBMs are more common in men aged over 50, and are more aggressive. Secondary GBMs arise from astrocytomas or other glial tumours, and may have better outcomes. So if my tumour was growing back in 2009 or earlier, then it may have been a lower grade tumour which changed into a GBM. Still not great, but better than a primary GBM. I'll do some more reading on the marvellous internet, when I get the energy.
Wishing you all love, peace, and health.
Tuesday, 12 November 2013
Dexamethasone, side effects, and fighting on when you feel utterly drained and like crap.
Side Effects
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common- Agitation
- Anxiety
- Blurred vision
- Dizziness
- Headache
- Irritability
- Mood changes
- Nervousness
- Numbness or tingling in the arms or legs
- Swelling of the fingers, hands, feet, or lower legs
- Trouble thinking, speaking, or walking (mixing up words in my case)
- Decreased vision
- Dry mouth
- Facial hair growth in females (light hair on sides of face)
- Fatigue
- Full or round face
- Heartburn and/or indigestion
- Increased hunger
- Increased thirst
- Increased urination
- Muscle pain or tenderness
- Muscle wasting or weakness
- Nausea
- Pain in back, ribs, arms, or legs
- Sleeplessness
- Trouble sleeping
- Unusual tiredness or weakness
- Vision changes
- Thinning of the scalp hair